Prostate pathology outlines
Maintenance between March 11 and 12 may cause some brief downtime. We apologize for any inconvenience!
This review article focuses on prostate carcinoma and underscores changes in the prostate chapter as well as those made across the entire series of the 5th edition of WHO Blue Books. Evolving and unsettled issues related to grading of intraductal carcinoma of the prostate and reporting of tertiary Gleason pattern, the definition and prognostic significance of cribriform growth pattern, and molecular pathology of prostate cancer will also be covered in this review. The publication of WHO Classification of Urinary and Male Genital Tumors 5th Edition marks another major milestone in the field of genitourinary GU pathology and is the culmination of scientific advancements in recent years built upon the 4th edition published in The new edition of this authoritative reference book provides a comprehensive update on tumor classification in the same modular fashion as the previous edition with the addition of several new sections for each disease entity, including cytology, diagnostic molecular pathology, essential and desirable diagnostic criteria, and staging. This review article highlights salient changes made to the prostate chapter as we have gained better understanding of the etiology, pathogenesis, and molecular pathology of prostate cancer.
Prostate pathology outlines
Maintenance between March 11 and 12 may cause some brief downtime. We apologize for any inconvenience! Page views in 7, Cite this page: Sanguedolce F. Nonspecific granulomatous prostatitis. Accessed March 11th, Essential features. Mixed, mostly chronic granulomatous inflammation epithelioid histiocytes, giant cells, lymphocytes, plasma cells and other inflammatory cells No specific etiology can be established on the basis of clinical and serological findings. ICD N Y - other specified inflammatory and other diseases of the prostate includes granulomatous prostatitis. Prominent inflammatory reaction to extravasated prostatic fluid containing bacterial toxins and cell debris within the prostate.
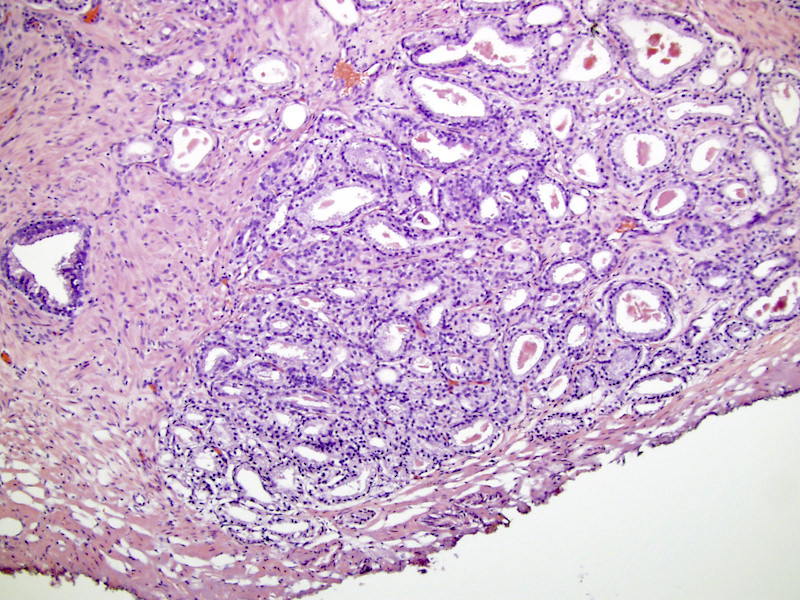
There should be no intervening stroma or mucin separating individual or fused glandular structures. This review article highlights salient changes made to the prostate chapter as we have gained better understanding of the etiology, pathogenesis, and molecular pathology of prostate cancer. Cribriform Growth Pattern Various neoplastic and non-neoplastic lesions in the prostate can have cribriform morphology, prostate pathology outlines, including central zone glands, clear cell cribriform hyperplasia, basal cell hyperplasia, cribriform HGPIN, AIP, IDC-P, and invasive cribriform prostate pathology outlines.
Maintenance between March 11 and 12 may cause some brief downtime. We apologize for any inconvenience! Page views in Cite this page: Matoso A. Accessed March 11th, Usually located in posterolateral soft tissue outside of prostate Seen in radical prostatectomy specimens and rarely in prostate needle biopsies, or in smooth muscle of bladder neck in transurethral resections of prostate or bladder.
Federal government websites often end in. The site is secure. This review focuses on histopathological aspects of carcinoma of the prostate. Markers detected by immunohistochemistry on tissue sections can support a diagnosis of adenocarcinoma that is primary in the prostate gland or metastatic. Histological grading of adenocarcinoma of the prostate, including use of the International Society of Urological Pathology ISUP modified Gleason grades and the new grade groups, is one of the most powerful prognostic indicators for clinically localized prostate cancer, and is one of the most critical factors in determination of management of these patients. The histopathological assessment of hematoxylin and eosin-stained tissue sections and, frequently, the detection of molecular markers by immunohistochemistry are critical for diagnosing, characterizing, and managing prostate cancer. The most common prostatic parenchymal tissue samples examined in surgical pathology laboratories in the United States are, in order, gauge needle cores, transurethral resections, radical prostatectomy specimens, open simple or enucleation prostatectomy specimens uncommon , and fine-needle aspirates rare. Needle core biopsies and fine needle aspirates may be used to diagnose metastatic prostate cancer. Prostate cancer indicates a malignant neoplasm of the prostate. The vast majority of these malignant neoplasms are of epithelial origin and differentiation, and are carcinomas.
Prostate pathology outlines
Return to the tutorial menu. The male prostate gland is located below the bladder. The seminal vesicles are located posterior to the prostate. The urethra exits from the bladder and traverses the prostate before exiting to the penile urethra. The normal prostate is composed of glands and stroma. The glands are seen in cross section to be rounded to irregularly branching. These glands represent the terminal tubular portions of long tubuloalveolar glands that radiate from the urethra. The glands are lined by two cell layers: an outer low cuboidal layer and an inner layer of tall columnar mucin-secreting epithelium. These cells project inward as papillary projections.
Harrisbteeter hours
Microscopic histologic description. MYB-NFIB gene fusion in prostatic basal cell carcinoma: clinicopathologic correlates and comparison with basal cell adenoma and florid basal cell hyperplasia. The proportion of cases that including or excluding IDC-P would have changed the grade in these studies is very small and would not have any significant impact. However, we cannot answer medical or research questions or give advice. The new edition of WHO Blue Book acknowledges these dissimilarities but does not endorse either position because the overall evidence is insufficient, and both positions are mainly based on consensus opinions Squamous carcinomas: adenoid cystic basal cell carcinoma adenosquamous carcinoma squamous cell carcinoma. Varma M, Epstein JI. Historical and contemporary perspectives on cribriform morphology in prostate cancer. PIN-like adenocarcinoma showing acinar A, x and ductal C, x morphology with flat or tufted architecture. Negative staining.
We can connect you with trained cancer information specialists who will answer questions about a cancer diagnosis and provide guidance and a compassionate ear.
Varma M, Epstein JI. However, stromal tumors of the prostate, thought to originate from prostate stromal cell proper, and treatment-related neuroendocrine prostatic carcinoma, are still included in the prostate chapter due to their uniqueness to the prostate, and distinctive biological and clinical characteristics as well as therapeutic implication for the latter. Usually located in posterolateral soft tissue outside of prostate Seen in radical prostatectomy specimens and rarely in prostate needle biopsies, or in smooth muscle of bladder neck in transurethral resections of prostate or bladder. Definition of Cribriform Glands. Large cribriform growth pattern identifies ISUP grade 2 prostate cancer at high risk for recurrence and metastasis. Jerasit Surintrspanont 1 , 2 and Ming Zhou 2. Immunohistochemically, the high-grade NE component shows nuclear p53 staining in the majority of cases, thyroid transcription factor 1 TTF1 positivity in about half of the cases, and AR positivity in a small subset of tumors. While awaiting more evidence, ductal PCa remains a distinct type of PCa due to its more aggressive behavior compared to acinar PCa and the predilection for liver and lung metastases as well as brain, skin, testicular, and penile metastases on rarer occasions 2 , 6. Paneth cell—like differentiation. Am J Surg Pathol ; 40

0 thoughts on “Prostate pathology outlines”