Postpartum hemorrhage ati
Federal government websites often end in. Before sharing sensitive information, make sure you're on a federal government site.
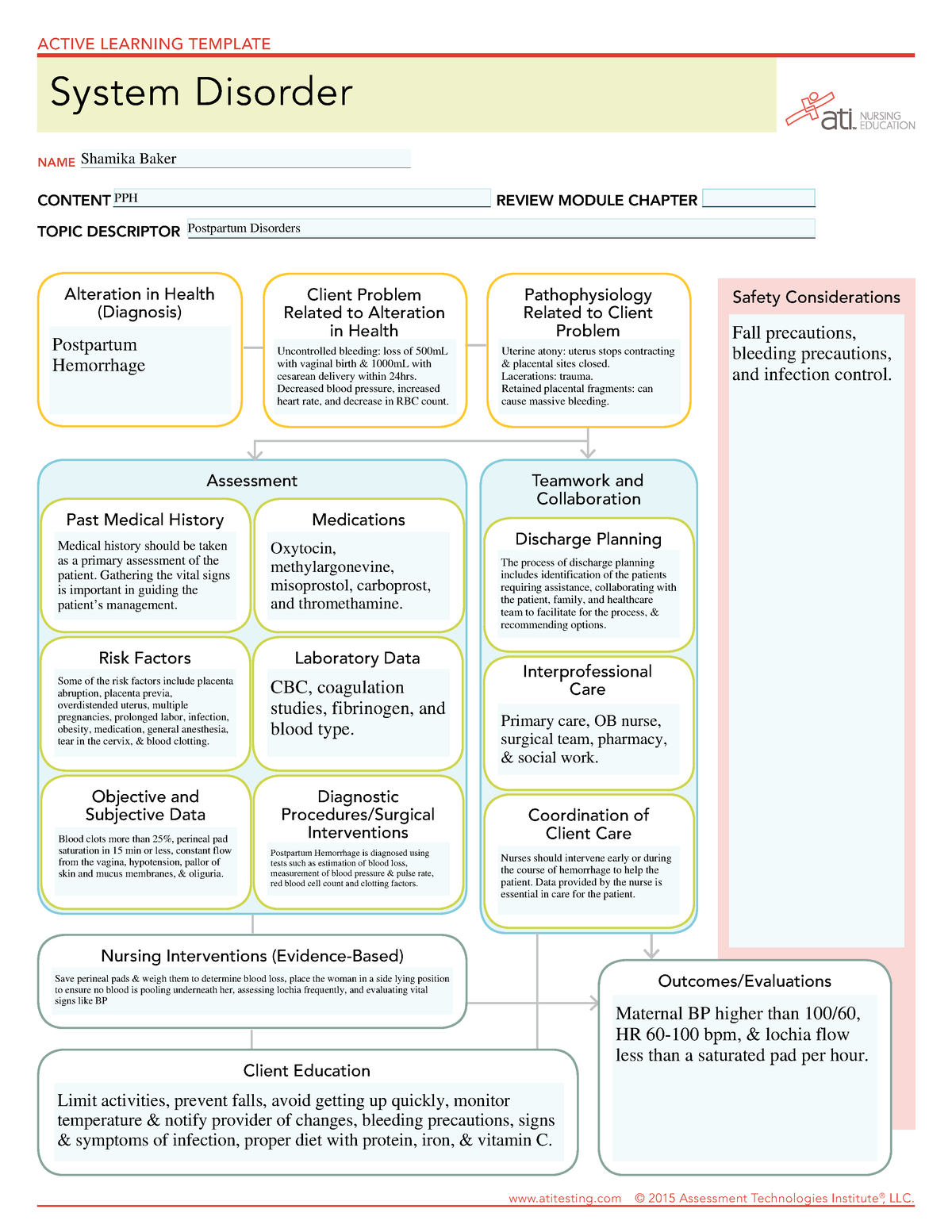
The postpartum period, a time of joy and celebration, can also present unexpected challenges, one of which is postpartum hemorrhage PPH. It accounts for the majority of the 14 million cases that occur each year. Postpartum hemorrhage is a significant and potentially life-threatening complication that requires prompt recognition, rapid intervention, and expert nursing care to ensure the well-being of the mother. As nursing professionals, understanding the risk factors, early signs, and evidence-based interventions for PPH is crucial in providing comprehensive care and support during this critical phase of the maternal journey. This article aims to serve as a comprehensive nursing guide to postpartum hemorrhage , delving into its causes, assessment techniques, and multidisciplinary management. You would not be able to miss out on the signs and symptoms of postpartum hemorrhage if you take a look at our list. Compliance to these medical interventions is critical for the survival of the patient.
Postpartum hemorrhage ati
.
It was helpful for me…. Supracervical hysterectomy may be performed alternately as a faster surgery with potentially fewer complicated risks.
.
The postpartum period, a time of joy and celebration, can also present unexpected challenges, one of which is postpartum hemorrhage PPH. It accounts for the majority of the 14 million cases that occur each year. Postpartum hemorrhage is a significant and potentially life-threatening complication that requires prompt recognition, rapid intervention, and expert nursing care to ensure the well-being of the mother. As nursing professionals, understanding the risk factors, early signs, and evidence-based interventions for PPH is crucial in providing comprehensive care and support during this critical phase of the maternal journey. This article aims to serve as a comprehensive nursing guide to postpartum hemorrhage , delving into its causes, assessment techniques, and multidisciplinary management. You would not be able to miss out on the signs and symptoms of postpartum hemorrhage if you take a look at our list. Compliance to these medical interventions is critical for the survival of the patient.
Postpartum hemorrhage ati
Complications of postpartum hemorrhage are listed in Table 1 3 , 6 , 7 ; these range from worsening of common postpartum symptoms such as fatigue and depressed mood, to death from cardiovascular collapse. This review presents evidence-based recommendations for the prevention of and appropriate response to postpartum hemorrhage and is intended for physicians who provide antenatal, intrapartum, and postpartum care. Risk factors for postpartum hemorrhage are listed in Table 2. The most effective strategy to prevent postpartum hemorrhage is active management of the third stage of labor AMTSL. AMTSL also reduces the risk of a postpartum maternal hemoglobin level lower than 9 g per dL 90 g per L and the need for manual removal of the placenta. Based on existing evidence, the most important component is administration of a uterotonic drug, preferably oxytocin. An alternative to oxytocin is misoprostol Cytotec , an inexpensive medication that does not require injection and is more effective than placebo in preventing postpartum hemorrhage. The benefits of controlled cord traction and uterine massage in preventing postpartum hemorrhage are less clear, but these strategies may be helpful. Diagnosis of postpartum hemorrhage begins with recognition of excessive bleeding and targeted examination to determine its cause Figure 1 6. Cumulative blood loss should be monitored throughout labor and delivery and postpartum with quantitative measurement, if possible.
Munch meaning in bengali
Compliance to these medical interventions is critical for the survival of the patient. Identifying high-risk patients before delivery is one of the most important factors in preventing morbidity and mortality associated with PPH. Uterine compression sutures may also be used as a treatment for atony. Coagulation parameters during the course of severe postpartum hemorrhage: a nationwide retrospective cohort study. Indian J Anaesth. Assess the condition of the uterus. A peripartum hysterectomy is associated not only with permanent sterility but also increased surgical risk with a higher risk of bladder and ureteral injury. It is important to keep an accurate count of anything placed in the uterus to prevent retained foreign bodies. Disclosure: Radia Jamil declares no relevant financial relationships with ineligible companies. This was redefined by the American College of Obstetrics and Gynecology in , and the current definition is cumulative blood loss greater than mL with signs and symptoms of hypovolemia within 24 hours of the birth process, regardless of the route of delivery. Continuous assessment of vital signs and ongoing estimation of total blood loss is an important factor in ensuring safe care of the patient with PPH. Towards a universal definition of postpartum hemorrhage: retrospective analysis of Chinese women after vaginal delivery or cesarean section: A case-control study. Thank you so much…. Antifibrinolytic drugs for treating primary postpartum haemorrhage. Describe the presentation of a patient with postpartum hemorrhage.
This topic will present an overview of major issues relating to PPH. Clinical use of specific medical and minimally invasive interventions, and surgical interventions at laparotomy, for management of PPH are discussed separately. See "Postpartum hemorrhage: Medical and minimally invasive management" and "Postpartum hemorrhage: Management approaches requiring laparotomy".
Uterine artery embolization may be considered in a stable patient with persistent bleeding. Acute Postpartum Hemorrhage - StatPearls. Postpartum hemorrhage is the leading cause of morbidity and mortality in childbirth. Deterrence and Patient Education Preventative techniques can be used in patients to prevent atony and PPH, including active management of the third stage of labor with oxytocin administration, uterine massage, and umbilical cord traction. Correct and timely institution of treatment can vastly improve patient outcomes. Marianne Belleza, R. This activity reviews the causes of postpartum hemorrhage and highlights the role of the interprofessional team in the management of these patients. If there is not an intrauterine balloon readily available, the uterus may be packed with gauze, or multiple large Foley catheters may be placed concurrently. Introduction Obstetric hemorrhage is the most common and dangerous complication of childbirth. Assess lochia frequently to determine if the amount discharged is still within the normal limits. Prognosis Postpartum hemorrhage is a leading cause of maternal and fetal morbidity in the United States. The B-Lynch suture technique, the most commonly performed among the compression sutures, physically compresses the uterus looping from the cervix to the fundus. Administration of Pitocin.

I doubt it.