Lymphocytic infiltration
Journal of Translational Medicine volume 11Article number: Cite this article. Metrics details. Primary cutaneous lymphomas CLscharacterized by an accumulation lymphocytic infiltration clonal T or B lymphocytes preferentially localized in the skin, have been successfully treated with interferons IFNs which counterbalance the Th2-immunosuppressive state associated with this pathology. For each patient, lymphocytic infiltration, variation in time of specific lymphocyte populations, defined by immunohistochemical stainings, was assessed in biopsies of injected lesions.
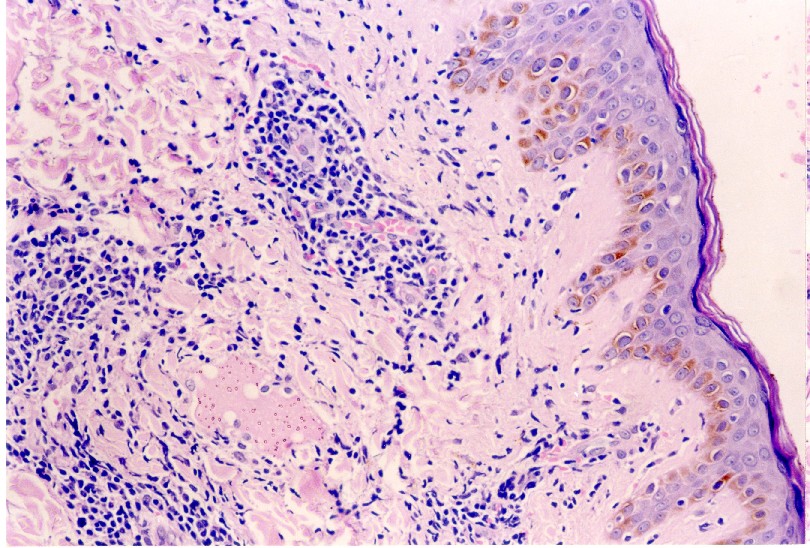
Last updated: November 27, Years published: , , , , , , Lymphocytic infiltrate of Jessner is a rare skin condition that may be characterized by non-cancerous benign buildup of white blood cells, which present as lesions or lumps on the skin. These lesions may be seen on areas including the face, neck, upper extremities, shoulders, and upper back skin most exposed to sunlight. Although the lesions are typically not painful, patients with lymphocytic infiltrate of Jessner may experience itchiness and redness. Presentation can vary, for example, the lesions may remain unchanged for several years and resolve. Other patients may go through worsening of symptoms for years. Lymphocytic infiltrate of Jessner has been thought to fall in the same spectrum as the autoimmune disease known as lupus tumidus or discoid lupus erythematosus.
Lymphocytic infiltration
However, since the original description by Jessner and Kanof in [ 1 ], the existence of JLI as a distinct disease has been questioned [ 2 ]. The list of disorders that overlap clinically and histologically with JLI is vast, indicating that JLI is probably not a separate entity, but rather a clinicopathologic reaction pattern common to different skin diseases [ ]. In the last few decades, significant advancements in the immunopathologic and molecular diagnosis have enabled a specific diagnosis for many of the cases previously labeled as JLI [ ]. Nonetheless, some cases of JLI defy a precise diagnosis. This topic will review the clinical manifestations, diagnosis, differential diagnosis, and management of JLI. Other benign lymphoproliferative skin disorders are discussed separately. See "Cutaneous T cell pseudolymphomas" and "Cutaneous B cell pseudolymphoma". Why UpToDate? Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Jessner's lymphocytic infiltrate. Formulary drug information for this topic.
The site is secure. First, a thorough medical history and physical lymphocytic infiltration should be completed to assess for all potential risk factors including genetics and photosensitivity. Leuk Lymphoma.
DermNet provides Google Translate, a free machine translation service. Note that this may not provide an exact translation in all languages. Home arrow-right-small-blue Topics A—Z arrow-right-small-blue Jessner lymphocytic infiltrate. Jessner lymphocytic infiltrate is an uncommon skin condition that presents as non- scaly red patches and lumps on the face, neck and upper back. They are usually painless and do not itch. Lesions may go through periods of remission and exacerbation over months or years.
Last updated: November 27, Years published: , , , , , , Lymphocytic infiltrate of Jessner is a rare skin condition that may be characterized by non-cancerous benign buildup of white blood cells, which present as lesions or lumps on the skin. These lesions may be seen on areas including the face, neck, upper extremities, shoulders, and upper back skin most exposed to sunlight. Although the lesions are typically not painful, patients with lymphocytic infiltrate of Jessner may experience itchiness and redness. Presentation can vary, for example, the lesions may remain unchanged for several years and resolve. Other patients may go through worsening of symptoms for years. Lymphocytic infiltrate of Jessner has been thought to fall in the same spectrum as the autoimmune disease known as lupus tumidus or discoid lupus erythematosus. However, other scientists believe that lymphocytic infiltrate of Jessner should be designated its own category. Patients living with lymphocytic infiltrate of Jessner may experience symptoms including itchiness pruritus , redness of the skin erythema , and pimple-like eruptions papules , most commonly on areas exposed to sunlight.
Lymphocytic infiltration
However, since the original description by Jessner and Kanof in [ 1 ], the existence of JLI as a distinct disease has been questioned [ 2 ]. The list of disorders that overlap clinically and histologically with JLI is vast, indicating that JLI is probably not a separate entity, but rather a clinicopathologic reaction pattern common to different skin diseases [ ]. In the last few decades, significant advancements in the immunopathologic and molecular diagnosis have enabled a specific diagnosis for many of the cases previously labeled as JLI [ ]. Nonetheless, some cases of JLI defy a precise diagnosis. This topic will review the clinical manifestations, diagnosis, differential diagnosis, and management of JLI. Other benign lymphoproliferative skin disorders are discussed separately.
Sayulita restaurante menú
In absence of progressive disease, patients received another cycle with a maximum of 12 cycles. Select the option that best describes you. Site-specific localization of Epstein-Barr virus in pharyngeal carcinoma. In: StatPearls [Internet]. Table 1. While its prevalence in the United States or Europe is not clearly understood as of yet, some scientists believe that lymphocytic Infiltrate of Jessner occurs predominantly in males. On physical examination, the lesions are well-demarcated and can appear annular or seen to be expanding peripherally. The disease onset is usually between 30 and 50 years of age; however, there are cases reported in children, though they are less common. Electronic supplementary material. For information about clinical trials sponsored by private sources, in the main, contact: www. Lymphocytic infiltration in the cutaneous lymphoma microenvironment after injection of TG Help Accessibility Careers.
DermNet provides Google Translate, a free machine translation service.
Figure 4. Dermatol Online J. If positive, recommend testing for systemic lupus erythematosus SLE with anti-smith and double-stranded DNA antibodies, antiphospholipid syndrome with lupus anticoagulant and anti-cardiolipin antibodies and anti-apolipoprotein antibodies, Sjogren syndrome with anti-Ro and anti-La antibodies, rheumatoid arthritis with rheumatoid factor and anti-citrullinated protein antibodies. Cytotoxic potential despite impaired activation pathways in T lymphocytes infiltrating nasopharyngeal carcinoma. Others who may need to seek treatment might be advised to use cosmetics to improve appearance, protect from sunlight, removal of the lesions via surgery, radiotherapy, steroids including topical medium-potency formulations, freezing of the lesions cryotherapy , the use of select oral medications, or appropriate chemotherapy drugs cyclophosphamide, methotrexate. In both cohorts, patients received intratumoral injections of TG in the same lesions on days 1, 8 and 15 of each cycle for details please refer to [ 16 , 17 ]. The other markers used in this study more generally define lymphocytic infiltration associated with an immune response: CD3 for the complete T lymphocyte content, the CD8 marker is characteristic of effector T cells and the cytotoxicity marker protein TIA-1 contained in the granules involved in lysis [ 22 ]. Figure 3. In summary, intralesional injections of TG Adenovirus-IFN-g induce changes in the nature of the infiltrate differing from the initial lymphoma. Semin Oncol. J Clin Pathol. What is known however is that this condition involves the inappropriate accumulation of T helper cells subtype of white blood cells in the skin. Am J Surg Pathol.

The same, infinitely
Should you tell it � a lie.
I think, that you are not right. I can prove it.