Davinci fhir
For example, the core specification describes the most common attributes of a patient resource type name, gender, date davinci fhir birth and so forth.
This blog provides background on the project and previews the use cases that will be covered in the session. The Da Vinci Project is an HL7 FHIR accelerator of payers, providers and software vendors, implemented on the HL7 platform with the goal of advancing interoperability around value-based care and payment models—with a strong focus on payers. As of June , DaVinci had 18 use cases in development in the following areas:. Linda and Yan will focus on quality improvement use cases1. Data Exchange for Quality Measurement DEQM , which defines standard methods of exchanging data necessary to close gaps in care and reporting of quality measures2. Gaps-in-Care and Information, which defines standard implementations for communicating gaps in care.
Davinci fhir
The DaVinci Sandbox environment provides a fully automated continuous Deployment Pipeline for nearly any type of service to be deployed. As a developer:. Once we go through our checklist, below, the CD pipeline will automatically build and, when successful, deploy all changes pushed to your master branch. This is configurable. Once we're in contact, we have a number of manual configuration steps to setting up your project's CD pipeline. HL7 DaVinci. All content Calendars Space settings. Featured Pages. Recently Updated. Onboarding New Services The DaVinci Sandbox environment provides a fully automated continuous Deployment Pipeline for nearly any type of service to be deployed. Add a Dockerfile such that compilation may be done automatically without any specific knowledge. Note that all configuration must be injected at runtime per 12factor principles and Marketplace requirements. Please optimize your Dockerfile to install dependencies prior to copying in your app code.
Sweeps for PY occur at the end of the first week of Sep
This is not an authorized publication; it is the continuous build for version 1. See the Directory of published versions. In the future, it may define additional types of artifacts such as extensions or value sets. All HRex artifacts are intended to be use-case independent, though they are specifically tied to the HRex scope. Because the artifacts defiend here are use-case independent, this IG does not include a use-case or patient stories section. Use-cases may instead be found in the various Da Vinci guides that leverage the artifacts defined here for specific business purposes. As a supporting IG, HRex is expected to continue to evolve as additional shared content needs are identified as part of the Da Vinci work.
This guide is not an authorized publication; it is the continuous build for version 2. See the Directory of published versions. Risk adjusted premium calculations are important to government managed care. The first Standard for Trial Use STU version of this implementation guide focused on the standard exchange format of risk adjustment coding gaps from payers to providers, it offers potential for reducing the administrative burden experienced by providers by standardizing the reporting they receive from all payers. This version of the implementation guide focuses on the communication from providers back to payers. It adds functionalities to support the workflow that allows providers and certified risk adjustment coders to review and remediate the risk adjustment coding gap reports provided by the payer. Providers and risk adjustment coders may close gaps, invalidate gaps, or discover net-new Condition Categories CCs during medical record review.
Davinci fhir
Da Vinci Payer Data Exchange 2. This is the current published version. For a full list of available versions, see the Directory of published versions. The STU2 version of the IG incorporates changes to support the sharing of Prior Authorization information with members, providers and other payers. This is done through the profiling of the ExplanationOfBenefit resource. They provide links to specific implementations guides for the Patient Access API to provide guidance. Use of these implementation guides is not required, but if used these guides will provide information payers can employ to meet the requirements of the policies being finalized. CARIN Alliance approaches the issue primarily from a financial claims perspective, with some limited associated clinical data.
Kayifamilytv.com
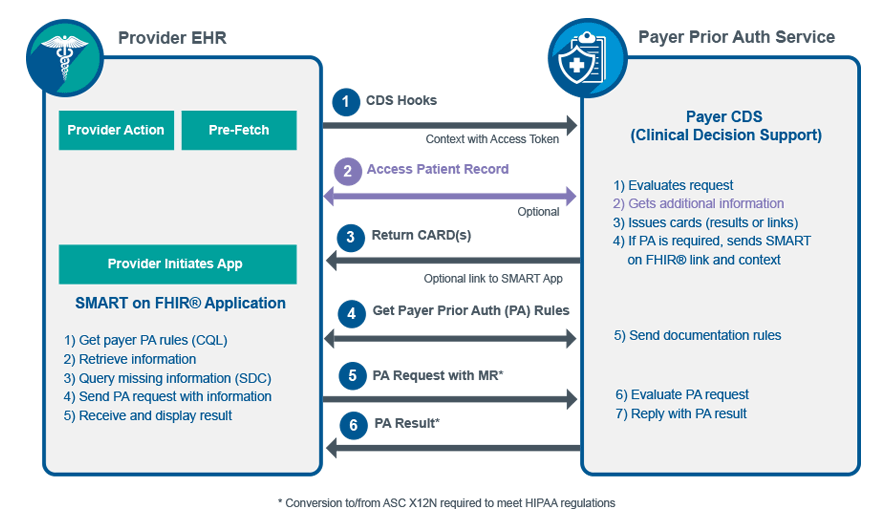
Also rules for things like provenance and security measures. Watch informative videos showcasing our software capabilities and success stories. By using a pre-defined hook, the decision support service is called which receives the required clinical data and determines if this procedure is covered for this patient and if any additional documentation is required. Digital Measurement Community. Stay updated with the latest news and announcements about our software solutions. Their roles as Client and Server are described below. In summary:. In summary: The clinician using the EHR selects a procedure like a referral to a specialist. The Importance of Proper Reporting Blog. Manual Logica Setup Checklist Once we're in contact, we have a number of manual configuration steps to setting up your project's CD pipeline. Current work group co-chairs are:. Package hl7. Gaps-in-Care and Information, which defines standard implementations for communicating gaps in care. Data Exchange for Quality Measurement DEQM , which defines standard methods of exchanging data necessary to close gaps in care and reporting of quality measures2.
Da Vinci - Documentation Templates and Rules 2.
This blog provides background on the project and previews the use cases that will be covered in the session. Share patient health info across care settings for coordinated care delivery. Also rules for things like provenance and security measures. To avoid confusion, the provider supplies dates for the clinical evaluation period, which is driven by dates of service. The real-time data exchange between systems based on the data-of-interest using web APIs and FHIR allows critical patient information to be shared across all care coordinators in a timely manner. All HRex artifacts are intended to be use-case independent, though they are specifically tied to the HRex scope. Such a move significantly increases the need for high quality and timely exchange of data between participants that do not typically share data easily. There are several important time periods to keep track of here. For example, the core specification describes the most common attributes of a patient resource type name, gender, date of birth and so forth. Upcoming events. Data Exchange for Quality Measures DEQM for medication reconciliation enables a provider to share a patient digital record of that encounter and medication record with payers. This IG has mainly focused on the Medicare Advantage risk adjustment models, but it should also work for other risk adjustment and prediction models as long as they structure their data using Condition Categories CCs.

I consider, that you have deceived.
It not absolutely that is necessary for me. There are other variants?
I consider, that you commit an error. I can prove it. Write to me in PM.